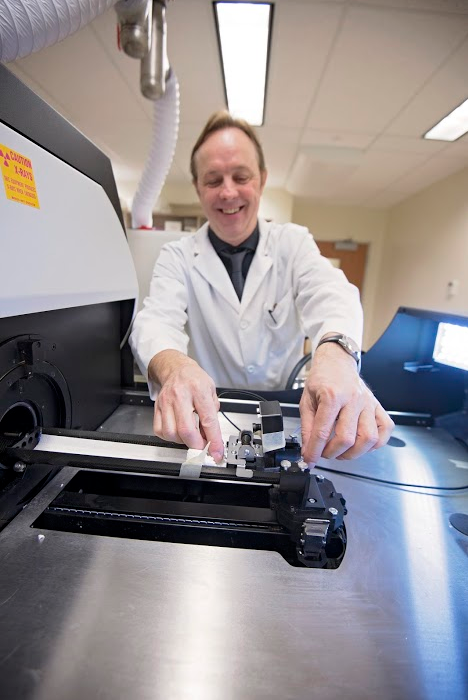
Associate professor Michael Doschak setting up the in vivo micro-Computed Tomography imager that is being used to measure improvements in bone mineral density after treatment with Dr. Doschak's novel bone-seeking drugs.
Michael Doschak, an associate professor in the Faculty of Pharmacy and Pharmaceutical Sciences, is embarking on a bold expedition. He recently received a Canadian Institutes of Health Research (CIHR) Proof of Principle - Phase 1 Grant for his project titled "Bone-Seeking Iron Oxide Nanoparticles for Imaging Bone Metabolism." This project will study how "diagnosing metabolic bone disease at an early stage plays a vital role in the success of treatment and management of diseases such as osteoporosis, Paget's disease and osteoarthritis, and the accurate diagnosis of overuse bone shin splints, or even metastatic bone cancers."
Doschak will conduct the translational research with the help of collaborators Richard Thompson, associate professor in biomedical engineering, and Jacob Jaremko, assistant professor in radiology and diagnostic imaging, both with the Faculty of Medicine & Dentistry at the University of Alberta.
Somewhat like Star Trek's Dr. McCoy using 23rd-century medicine, Doschak leads his team of graduate students and post-docs on a mission to "improve to improve quality of life and reduce side-effects for patients through the technology of bone drug discovery."
According to Doschak, "bone drug delivery involves finding a cellular mechanism or process that will pull the drug preferentially into bone like a building block, to treat the bone cells directly, while avoiding other body organs and tissues." "The problem right now is that drugs intended to treat bone conditions also inadvertently 'poison' the entire body, when in fact we want that drug to work directly on bone cells alone. And that can sometimes lead to unwanted side-effects" says Doschak. "To address that shortcoming, we have developed a bone-targeting platform of drugs and contrast agents by decorating superparamagnetic iron oxide nanoparticles (SPIONs) with bone-seeking bisphosphonate (BP) drug tethers." This method has "shown that bone active drugs and BP-SPION imaging tracer will localize preferentially at sites of dynamic bone turnover, and can be detected with non-invasive magnetic resonance imaging (MRI), to highlight and treat adaptive bone pathology without the need for ionizing radiation."
At present, X-rays or nuclear medicine bone scans are used to diagnose bone pain. "X-rays only give you a static snapshot of the problem," says Doschak. "Often, the diagnosis will require a followup radioactive bone scan at a nuclear medicine facility, would increase the time to diagnosis and further involve systemic exposure of the patient to ionizing radiation."
Doschak's research aims to improve on those current methods to save patients both time and negative side-effects. "If an imaging tracer of bone turnover were visualized under MRI, then a single scan would provide significantly improved spatial resolution, zero exposure to ionizing radiation and the opportunity to image both soft tissue and the pattern of bone remodelling during the same clinical sitting."
Currently, there are no other imaging tracers of dynamic bone turnover that do not require some form of ionizing radiation component, be that from the radionuclide tracer itself or from the X-ray-based detection.
The research is currently being optimized at the bench with hopes of translation to clinical trials in sports medicine patients within the next 24 months. The CIHR grant allows Doschak to conduct important pre-clinical testing using micro-CT and MRI, to confirm that this bone drug delivery system will localize bone disease treatment.
So what does this mean for those who suffer from osteoporosis and osteoarthritis?
First, it may help reduce health-care costs-as Doschak notes, magnetic resonance imaging is cheaper and safer than radionuclide scans. And "unlike a radionuclide, the BP-SPION can be flushed down the sink. It's very safe. Every red blood cell in our body has iron oxide."
In addition, the non-radioactive bone diagnostic may open up new patient populations for access to things like bone scans, such as children having a BP-SPION-based MRI scan rather than being exposed to repeated X-rays. Doschak hopes to see the bone-seeking drug delivery platform validated for human use.
"Once we prove the value of this imaging tracer, the support will follow and we might be able to change outcomes for osteoporosis patients and improve their quality of life," says Doschak. "The first line of defence for these patients has been potent nitrogenated bisphosphonate drugs in high concentration, that have shown quite high toxicity with long-term use, resulting in brittle bone and severe dental side-effects. They keep the disease in check for the first five years, but now your risk of fracture is much greater and your bone is more brittle-it's a vicious circle.
"Our drugs will deliver peptide hormone drugs that send a strong message to bone cells, after which they break down into harmless amino acids and are recycled in your body."
Following the pre-clinical safety and efficacy studies, Doschak will file a clinical trial application with Health Canada and seek investor dollars to get the drug to the clinic. Initial findings have shown success for conditions like osteoporosis, and Doschak is hoping there will be benefits for cancer patients as well.
"Several common cancers such as prostate and breast cancer often metastasize to bone," he says. "One challenge is how to block this progression, because once the cancer gets to the bone, the patient suffers incredible pain."
Doschak's hope is to use the bone-seeking iron oxide nanoparticles to initially detect the bone metastases, while simultaneously delivering a drug payload to "protectively coat the bone surface and block the cells from attaching there."
"My hope is that this will also reduce the awful side-effects such as osteonecrosis of the jaw in cancer patients, and be further modified to help those suffering from osteoarthritis, by providing a targeted bone drug delivery approach."
