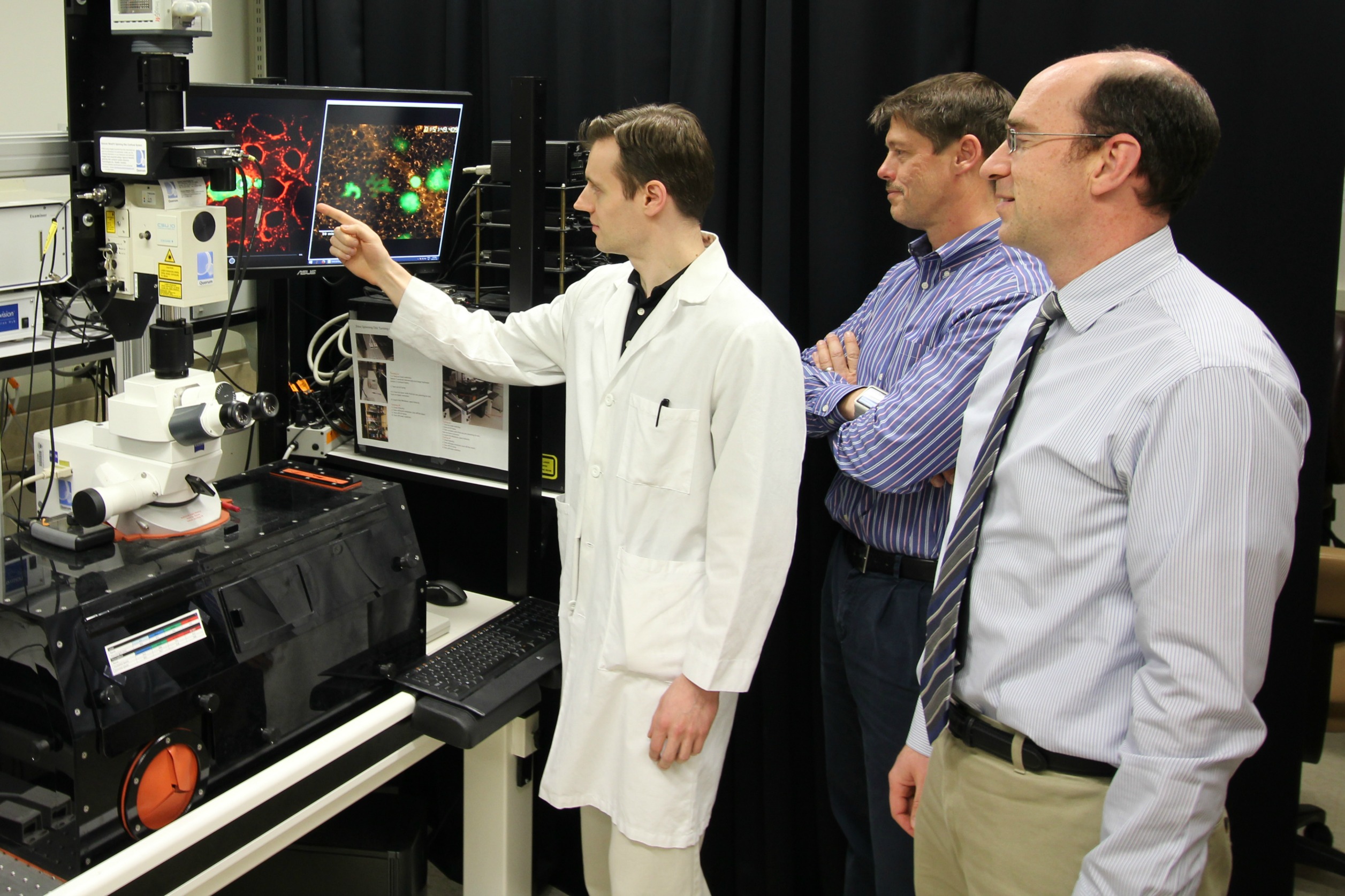
Researchers Robert Paproski, John Lewis and Roger Zemp co-authored a study that shows how focused ultrasound along with particles called nanodroplets can be used for the enhanced detection of cancer biomarkers in the blood.
Each year, thousands of Canadian men with prostate cancer undergo biopsies to help their doctors better understand the progression and nature of their disease. It provides vital, sometimes life-saving information, yet cancer researcher John Lewis knows it can be a difficult test to ask of anyone.
"Currently the best way to get information is through a biopsy, which involves pushing 12 needles through an organ the size of a walnut. As you might imagine, it's a very uncomfortable and invasive procedure," says Lewis, the Frank and Carla Sojonky Chair in Prostate Cancer Research at the University of Alberta and a member of the Cancer Research Institute of Northern Alberta. "Patients with low grade prostate cancer can decide not to get treatment and instead monitor the disease, but monitoring usually involves a biopsy every year or so. Many people opt for surgery instead of more biopsies. It is clearly something we need to improve upon."
A new innovation from the University of Alberta is promising to do just that through a relatively painless procedure. A study published in the journal Cancer Research describes the use of focused ultrasound along with particles called nanodroplets for the enhanced detection of cancer biomarkers in the blood. The research team, led by senior co-authors John Lewis and Roger Zemp, used the technique on tumours to cause extracellular vesicles to be released into the bloodstream, giving them large amounts of genetic material to analyze from drawing just a small sample of blood.
"With a little bit of ultrasound energy, nanodroplets phase-change into microbubbles. That's important because ultrasound can really oscillate these microbubbles," says Roger Zemp, professor of engineering at the U of A. "The microbubbles absorb of the ultrasound energy and then act like boxing gloves to punch the tumour cells and knock little vesicles off."
"That led us to detect some genes that were indicative of the aggressiveness of the tumour. That's potentially very powerful. You can get a genetic characterization of the tumour, but do it relatively non-invasively."
"Separately, the ultrasound and nanodroplets had very little effect," says Robert Paproski, first author of the study and a research associate working with Roger Zemp in the Faculty of Engineering. "But when we added the two together they had a very big effect. It allows us to detect roughly 100 times more vesicles than would normally be there, that are specific from the tumour."
The researchers say the technique is as accurate as using needles in a biopsy, with the ultrasound able to give them information about specific parts of a tumour. They add that genetic information can be used for personalized medicine - helping doctors know if a patient's tumour has a specific mutation which would then allow them to determine what medications would work best for treatment.
The team is pushing forward with strategies to further enrich the population of key vesicles released into the bloodstream through the technique, focusing on the biomarkers that are of the most importance. Lewis believes they can quickly progress the work to clinical trials, and from there to real world applications, thanks to the accessibility of the technology.
"Focused ultrasound systems are already used in the clinic. Microbubbles are already used in the clinic. So I think the movement of this into the clinic is relatively straightforward."
Meet our partners in innovation:
Prostate Cancer Canada is the leading national foundation dedicated to the prevention of the most common cancer in men through research, advocacy, education, support and awareness. As one of the largest investors in prostate cancer research in Canada, Prostate Cancer Canada is committed to continuous discovery in the areas of prevention, diagnosis, treatment, and support.