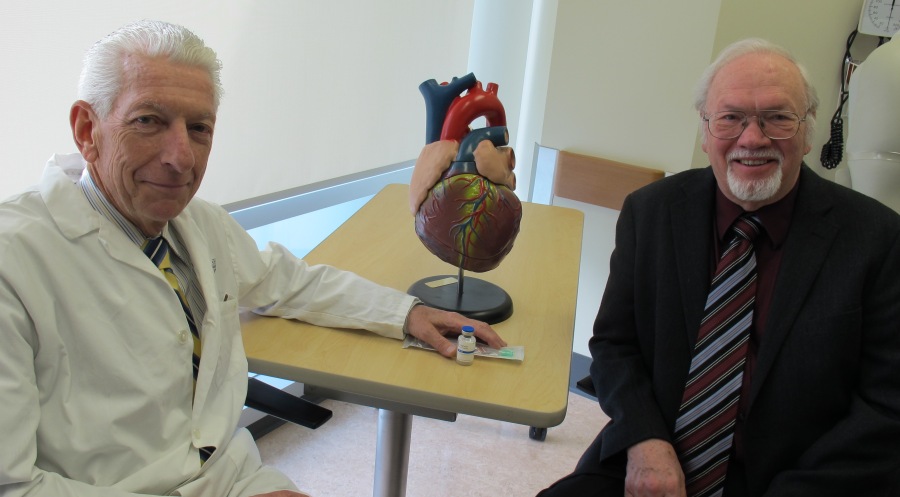
Paul Armstrong, left, poses with study participant Robert Harrison
(Edmonton) An international study involving about 1,900 patients from 15 different countries has found heart attack patients who receive clot-busting drugs in the first three hours post-heart attack, followed up with an angioplasty, do just as well as patients who only receive angioplasties within the three-hour window.
The international study was co-led by Faculty of Medicine & Dentistry researcher Paul Armstrong and his colleague, Frans Van de Werf from the department of Cardiovascular Sciences at the University of Leuven in Belgium. Their findings were published in the peer-reviewed journal, New England Journal of Medicine, on Sunday, at the same time as Van de Werf presented the highlights at the American College of Cardiology conference in San Francisco.
The study investigated whether one treatment approach was superior to the other - a topic that has been hotly contested in the cardiovascular medical field. Although angioplasty is considered a superior treatment if it can be delivered quickly, this is often difficult given the need for rapid access to specialty care and facilities.
Both treatments help open obstructed coronary arteries in patients who have just had a major heart attack. Clot-busting drugs can be given via needle and administered in an ambulance. Angioplasty uses a catheter to mechanically open the blocked coronary artery causing the heart attack and must be administered in tertiary care hospitals by specialists trained in the field. Only three such facilities exist in Alberta.
"Many have believed the angioplasty catheter-based therapy is superior," says Armstrong, a distinguished university professor with the Department of Medicine and a cardiologist with Alberta Health Services. "The challenge with this treatment is it needs to be provided very quickly by an expert team in a facility that has such experts available 24 hours a day, seven days a week. This is very difficult to achieve in many instances, and the resulting delay can lead to loss of valuable heart muscle and higher rates of death, shock and heart failure.
"There are many health-care sites around the world that don't have the luxury of these specialized sites. And in many countries, it can be challenging for patients to get to such facilities within three hours - due to long travel distances, heavy traffic, poor weather or other factors."
This discovery will be helpful to many patients who cannot access angioplasty rapidly and will change the way doctors treat and care for heart attack patients, Armstrong believes.
"Those who advocated the one-size-fits-all approach will be forced to rethink their proposition because we tested and delivered both treatments optimally in this study. Both treatments were delivered faster than anyone has done before and the results were clear - one treatment was just as good as the other.
"This study shows health-care workers they have two treatment options available, so they can use whichever is best - the right therapy for the right patient at the right time and the right place. It's also a wake-up call to health-care providers to pay attention to symptoms so patients are treated early and it emphasizes that ambulance and pre-hospital care is a critical part of making sure the patient has the best outcome possible."
Armstrong says it is widely known that the longer the delay to treatment after the onset of heart attack symptoms, the more severe the heart attack and the smaller the chance for the patient to survive.
Robert Harrison, 71, of Edmonton, took part in the study. He had a major heart attack two years ago on the Easter weekend. He received clot busting drugs in the ambulance, followed by an angioplasty within three hours.
"Speaking with my cardiologist and family doctor, I think the clot busting drugs saved my heart from having damage. I have no damage at all to my heart. I think my outcome would have been worse without the clot busting drugs."
The international trial involved 99 centres worldwide and 92 Canadians, including 67 from the Edmonton region and 25 from the Toronto area. The study examined how heart attack patients fared 30 days after one of the treatments - half of the patients were treated with a strategic approach with clot busting drugs within three hours, followed up by an angioplasty, while the other half had angioplasties within the three hours. Armstrong and his colleagues looked at the patients' mortality rates, and the likelihood of shock, heart failure and recurrent heart attack. During the study, the team discovered a slight increase in bleeding with the clot buster approach which was counterbalanced by a trend towards less shock and heart failure in those patients. The mortality rates were similar.
The official name of the study was the Strategic Reperfusion Early After Myocardial Infarction (STREAM) study.
Armstrong and his colleagues will continue their work with this study, exploring additional data about heart muscle damage, seeing how patients fared one year after treatment, and examining which patients fared the best long-term. They expect these results will be published in about one year.
The study was funded by Boehringer Ingelheim.